Acute Respiratory Distress Syndrome
Background
 Acute Respiratory Distress Syndrome (ARDS) is a life- threatening lung condition characterized by widespread inflammation, damage to the alveoli (air sacs), and impaired oxygen exchange. ARDS can be caused by various factors such as severe infections including SARS-Cov-2, pneumonia, aspiration, trauma, or inhalation of harmful substances. It often requires mechanical ventilation in an intensive care unit (ICU) setting. Despite advances in critical care, ARDS mortality rates remain high, ranging from 30% to 50%.
Acute Respiratory Distress Syndrome (ARDS) is a life- threatening lung condition characterized by widespread inflammation, damage to the alveoli (air sacs), and impaired oxygen exchange. ARDS can be caused by various factors such as severe infections including SARS-Cov-2, pneumonia, aspiration, trauma, or inhalation of harmful substances. It often requires mechanical ventilation in an intensive care unit (ICU) setting. Despite advances in critical care, ARDS mortality rates remain high, ranging from 30% to 50%.
ARDS due to all causes affects approximately 200,000 individuals in the US each year. The healthcare system and society bear substantial costs due to ARDS. Hospitalization costs for ARDS patients can range from $50,000 to $100,000 per case, considering intensive care unit (ICU) stays, mechanical ventilation, and other supportive treatments. The economic burden of ARDS includes direct medical costs associated with hospitalization, mechanical ventilation, and medication, which can range from tens of thousands to hundreds of thousands of dollars per patient. Additionally, the indirect costs related to disability, loss of productivity, and potential long-term healthcare needs further contribute to the overall economic impact. A study estimated that the mean cost per ARDS patient was $95,000 during the first year, with substantial variation depending on disease severity and complications. (Source: NIH – National Heart, Lung, and Blood Institute)
Current treatments for ARDS are primarily supportive, focusing on mechanical ventilation to maintain oxygenation and manage complications. However, these treatments have severe limitations. Ventilator-induced lung injury, barotrauma, brain injury leading to cognitive loss, and infection risks are common in ARDS patients, adding to the complexity of managing the condition. There is a critical need for novel therapies that can target the underlying pathophysiology of ARDS and improve patient outcomes.
ARDS specifically due to viral infections, such as influenza, SARS-CoV-2 (COVID-19), or other respiratory viruses, presents a particularly significant public health challenge. These viral infections can trigger a dysregulated immune response and widespread inflammation, leading to severe lung damage and respiratory failure.
The COVID-19 pandemic has highlighted the urgent need for effective treatments for viral-induced ARDS. Currently, supportive care measures, including oxygen supplementation and mechanical ventilation, are the mainstay of treatment. However, the morbidity and mortality rates associated with severe viral-induced ARDS remain high.
Current treatments for viral-induced ARDS, including ARDS due to COVID-19, are limited in efficacy. Antiviral therapies targeting the specific viral pathogen may help control viral replication but often fail to address the immune dysregulation and inflammation driving lung injury. Additionally, the development of antiviral resistance poses further challenges. Innovative therapies that can modulate the immune response, reduce inflammation, and promote lung repair are crucial to improving outcomes in viral-induced ARDS. Despite the progress in COVID-19 management, COVID-19-related hospitalizations and ICU stays remain a concern, and result in significant medical expenses, which can range from thousands to tens of thousands of dollars per patient, depending on the severity and length of hospitalization. (Source: JAMA Network)
The Theratome Solution
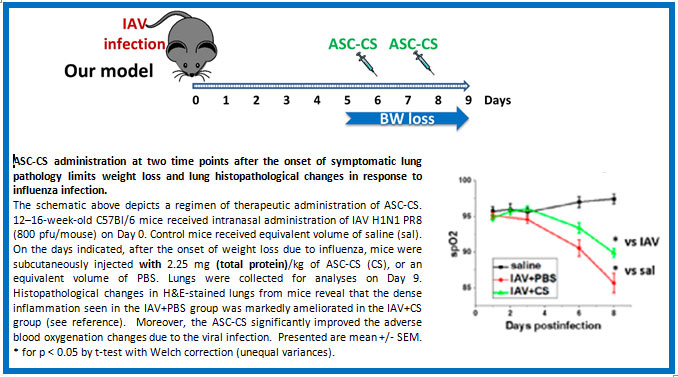
Our Secretome therapy has been shown to alleviate inflammation and promote lung tissue repair in ARDS patients. In addition to reducing lung injury, our product may also reduce secondary injury to brain, kidneys, and other organs that frequently occurs in ARDS. By delivering therapeutic biomolecules, including extracellular vesicles, growth factors, and cytokines, the Secretomes will help reduce inflammation, improve lung function and enhance patient outcomes. Uniquely, these products have been shown to elicit therapeutic immunomodulatory effects in animal models without reducing the host’s immune system ability to clear viral infection.