Stress Urinary Incontinence
Background
Urinary incontinence is an uncontrolled leakage of urine. It is often related to pelvic surgery, pregnancy, childbirth, and menopause. Globally, about 35% of the population over 60 years of age is estimated to be incontinent. It is more common in patients with obesity, diabetes, and depression.
There are four main types of incontinence:
- Urge incontinence due to an overactive bladder
- Stress incontinence due to a poorly functioning urethral sphincter muscle
- Overflow incontinence due to either poor bladder contraction or blockage of the urethra
- Mixed incontinence involving more than one factor listed above
While this disease can affect both men and women, it is most common in older women, particularly when post-partum; and in post-menopausal women whom have had multiple vaginal deliveries. Furthermore, sensory neural function relating to sexual sensation may be compromised in this setting.
Non-urologic causes include infection, medication of drugs, psychological issues and restricted mobility.
The Theratome Solution
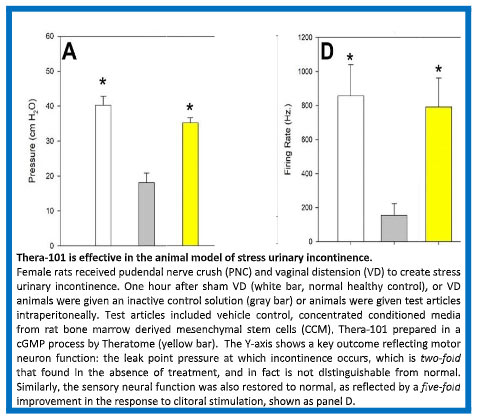
A collaboration of Theratome and Cleveland Clinic, supported by NIH through a non-dilutive STTR grant, demonstrated in well-accepted animal models of post-partum pudendal nerve injury that the use of Thera-101 manufactured under cGMP compliant conditions significantly increased nerve firing rate, improved reinnervation and accelerated recovery in stress urinary incontinence (SUI).
The study showed that the Secretome manufactured from adult stem cells, including both bone marrow-derived mesenchymal stem cells (MSCs) and adipose-derived mesenchymal stem cells (ASCs) would facilitate neuroregeneration leading to recovery of bladder control, as well as sensation in the genital region. This recovery was evident even when Secretome is delivered systemically.
The results of these studies demonstrated that both leak point pressure (LPP; a measure of bladder sphincter function) and spontaneous pudendal nerve activity were significantly decreased in the pudendal nerve crush (PNC) & vaginal distension (VD) rat models of SUI but were restored with MSC or Secretome treatment. Elastic fiber density in the urethra increased and changed in orientation with SUI in this rat model, with a greater increase in density of elastic fibers. Pudendal nerve fascicles were less dense and irregularly shaped with SUI but had reduced pathology. Thus, in this model, MSCs and their Secretome provide similar protective effects after pudendal nerve crush plus vaginal distension, suggesting that treatment with the cells themselves is not necessary, because the cells function through their secretions.
We have written and are currently refining a Phase II STTR proposal in consultation with the NIH. We anticipate that this will provide additional non-dilutive support to proceed to define an optimized route of delivery and dose-dependence of Thera-101 in this SUI model in order to prepare a clinical study for IND submission to FDA and translation of this promising therapy into clinical studies.
Competition
While physical therapy and medical devices can improve urinary incontinence, they most often are not curative. Surgery is also an option but has risks of complications.
Several medications are prescribed to treat urinary incontinence, including fesoterodine ($406 for 30 tablets, taken daily), tolterodine ($95 for 30 capsules, taken daily) and oxybutynin. However, medications are effective about 10% of the time and have systemic side effects.